CONVENTIONAL APPROACH
Cognitive Behavioural Therapy (CBT)
What is Cognitive Behavioural Therapy?
Cognitive Behavioural Therapy (CBT) is one of the most widely used forms of psychodynamic, evidence-based practice for improving mental health. It is a psycho-social intervention that works to alter unhelpful thoughts, beliefs, attitudes, and behaviours by improving emotional regulation through the development of targeted skills and strategies. It is a “short-term, structured, goal-focused, and action-oriented therapy” that helps individuals understand “the connection between mood, thoughts, behaviours and physical symptoms, and the relationship to the environment in which we live” (O’Neill, 2017, p. 253).
Source: Thrive Treatment
Measurement of a service users’ achievement of their goals is critical in calculating the efficiency of CBT. Therefore, careful assessment and monitoring of a service user’s progress is vital to the practice. One form of measuring progress is through worksheets and homework assignments as well capturing mood ratings/scores. Because the success of CBT is contingent upon an individual’s voluntary participation (Matthews et al., 2003), CBT utilizes homework assignments and additional reading materials to assist in the service user’s therapeutic growth in interventions such as cognitive restructuring, problem-solving, and mindfulness (Cully & Teten, 2008).
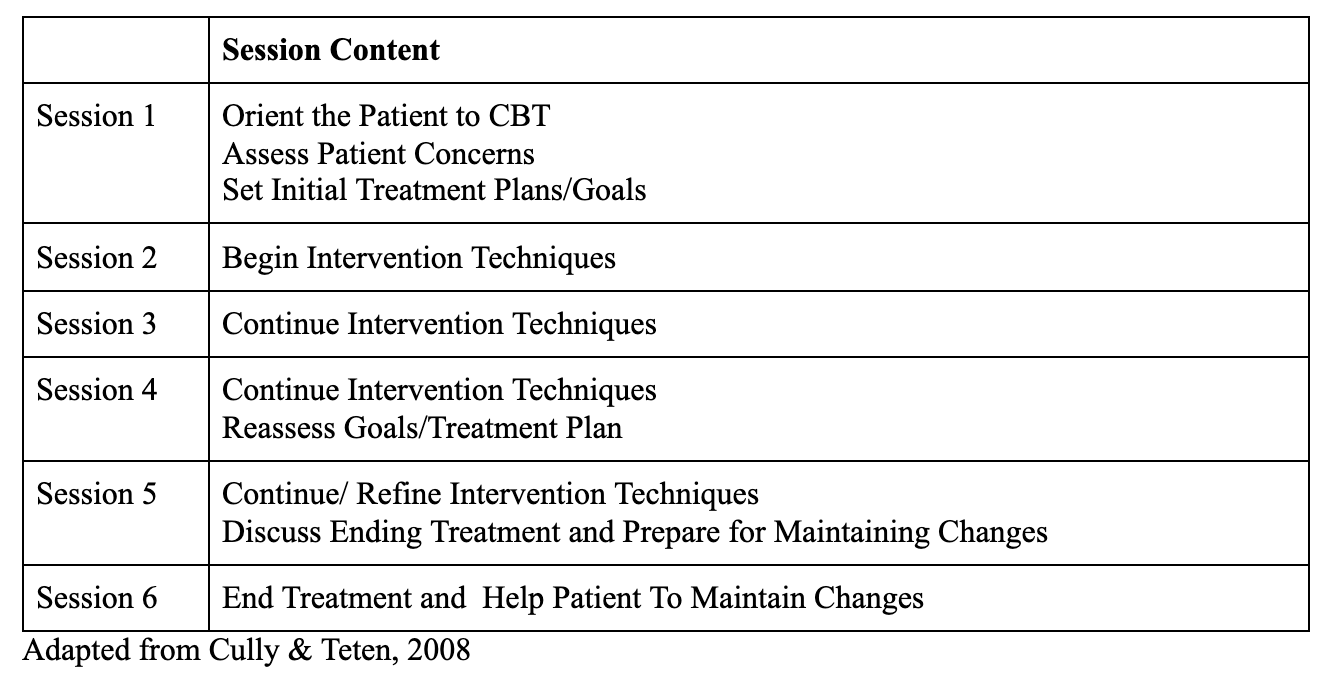
Through a collaborative process with a CBT therapist, service users develop strategies to replace dysfunctional core beliefs through 6-8 targeted sessions to address specific issues that they have identified as detrimental to their mental health. CBT is meant to be a brief intervention utilizing specific treatments for a limited number of sessions. While there is a range in duration, common consensus around CBT holds that a time-limited therapy may act as an additional incentive for patients and therapists to work efficiently (Cully & Teten, 2008; Payne, 2016; O’Neill, 2017). CBT is widely lauded in the mental health sector for not only its effectiveness in the treatment of many psychological disorders, but also for its position as a cost-effective method of intervention (O’Neill, 2017).
What are the origins of CBT?
In the 1970’s, Cognitive Behavioural Therapy was created as a product of the integration of two therapies: cognitive therapy and behavioural therapy (Miller, 2005). Cognitive therapy is derived from cognitive theory, which is an approach to psychotherapy that attempts to explain human behaviour through understanding thought processes and interpretations of life events. It argues that “our perceptions and interpretations of the world around us affect our behaviour as we learn” (Payne, 2016, p. 156).
Behavioural therapy was developed out of social learning theory, which states that learning is gained by modelling behaviour of those around us. Behavioural therapy aims to change potentially destructive or unhealthy behaviours through “conditioning” that will allow individuals to adopt new and healthy ways of interacting with their world (Payne, 2016). Cognitive behavioural therapy pulls from both methods to create an approach that attempts to change behaviours by focusing on and challenging the thoughts that create them.
What is the role of the social worker within CBT?
The role of the social worker in CBT is to provide a collaborative setting in which the service user has an active role in their treatment. A CBT therapist can provide methods for understanding and working through cognitive distortions; however the internal work and change processes are reliant on the service user’s ability to engage with the treatment.
Consequently, a strong therapeutic relationship that promotes mutual respect and trust is crucial. To create a meaningful and supportive relationship with a service user, authors Cully and Teten (2008) note that CBT therapists should seek to demonstrate empathy through validating a service user’s experiences, authenticity in their presentation and interactions, and demonstrating a positive regard by showing the service user the respect they deserve through non-judgement and commitment to their well-being.
“The therapeutic relationship in CBT is characterized by an active, directive stance by the therapist, high levels of emotional support, high levels of empathy and unconditional positive regard”
(Keijsers et al, 2000, p. 268; Brisebois & Gonzalez-Prendes, 2012, p. 24).
(Cully & Teten, 2008)
The emotional experiences that result from this therapeutic relationship can be integral to the service user’s progress and can lead to changes in cognition and their insight (Hardy et al., 2007).
Therefore, centering the empowerment and strengths of the service user are critical to the development of a strong therapeutic relationship and the success of CBT. The ultimate goal of the CBT therapist is to work with the service user to develop skills and strategies that allow them to manage their symptoms on their own (Brisebois & Gonzalez-Prendes, 2012). What are some strengths of CBT?
Adaptable to meet the needs of individuals
CBT uses a wide variety of methods to treat individuals with mental health issues utilizing interventions such as Dialectical Behaviour Therapy, Motivational Interviewing, and Mindfulness training.
Often these treatment methods will be used in conjunction with others. Each treatment plan identifies the particular behaviours and conscious processes that need to be targeted. This flexibility means that each individual’s treatment is specifically curated to meet their needs and stated goals.
Cost-effective, brief therapy with high rates of success
CBT models are widely used for their perceived low cost, structured sessions, and measurable outcomes. Research on CBT has shown that evidence-based care packages featuring CBT cost less and increase societal benefit, compared with care featuring medication (Myhr & Payne, 2006). For this reason, health professionals argue that CBT could produce significant cost savings to the Canadian government in conjunction with better mental health outcomes.
The brief nature of CBT (6-8 sessions) also produces a desirable quality: it is a relatively fast treatment method in a society with dramatically increasing rates of depression and anxiety (Smetanin et al., 2011), two common mental health concerns treated by CBT.
Further, CBT models highlight the importance of monitoring treatment processes to assess the success and efficacy of the intervention. As an evidence-based practice method of intervention, CBT provides measurable outcomes that are observable and tracked closely, making it the preferred method of treatment in many mental health organizations.
What does CBT look like in practice?
Step 1: Assessment
Assessments are used to:
Understand the service user and their current issues
Inform treatment and intervention techniques
Serve as a foundation for assessing progress during the treatment plan.
Step 2: Case Formulation
Draws on evidence about the particular problem and how it may be tackled
Proposes a model of what is happening to the service user and enables them to have a discussion with the CBT therapist about processes that are occurring, and strategize about how to tackle them
Sets goals with service user
Assesses service user’s concerns/difficulties
Establishes treatment plan
Identifies treatment obstacles
Source: Cully & Teten, 2008
Common CBT Interventions
Step 3: CBT Treatment Sequence
Utilizing information from Steps 1 and 2, implement a treatment plan and sequence that best fits the needs and goals of the service user
Potential Brief CBT Treatment Sequence
CBT Intervention Example: Cognitive Restructuring
Cognitive restructuring is a process in which a service user challenges and replaces negative thoughts and cognitive distortions. It aims to create more positive and functional thought habits and strategies to overcome irrational or maladaptive thoughts (Mills et al., 2008). Cognitive restructuring can include developing the skills to identify triggers that lead to negative emotions, gaining greater perspective on situations, and recognizing automatic thoughts and feelings (Bonfil & Wagage, 2020).
This technique is not simply about changing all negative thoughts to positive ones; rather, it emphasizes developing a perspective that can consider both positive and negative thoughts and outcomes. Further, it works to help service users choose to focus on thoughts that are most helpful in achieving their aims and that has less negative emotions attached (Bonfil & Wagage, 2020).
A Breakdown of Cognitive Restructuring (Bonfil & Wagage, 2020)
Step 1: Record the situation, thoughts, and feelings
Step 2: Pick one automatic thought from the list created
Step 3: Develop a different point of view about the situation
Consider:
What is the effect of believing this thought?
What would happen if I didn’t believe this thought?
What is the evidence supporting this thought?
What is the evidence against this thought?
Is there an alternative explanation?
What is the worst/best thing that could happen?
What can I do about this?
Step 4: Craft an alternative response